By Prince Agwu, Obinna Onwujekwe, Dina Balabanova and the Accountability in Action Research Team
Background
Despite anticorruption thrusts that have always been a part of the manifestos of successive governments in Nigeria, corruption has remained considerably high in the country. With corruption being common in many sectors of Nigeria, the country in the 2021 Corruption Perception Index (CPI), scored 24 of 100, making it the 154th most corrupt country out of 180 countries in the world, and among the 15 most corrupt countries in Africa. Disappointingly, the health sector continues to feature as among the top-5 corrupt sectors in the country.
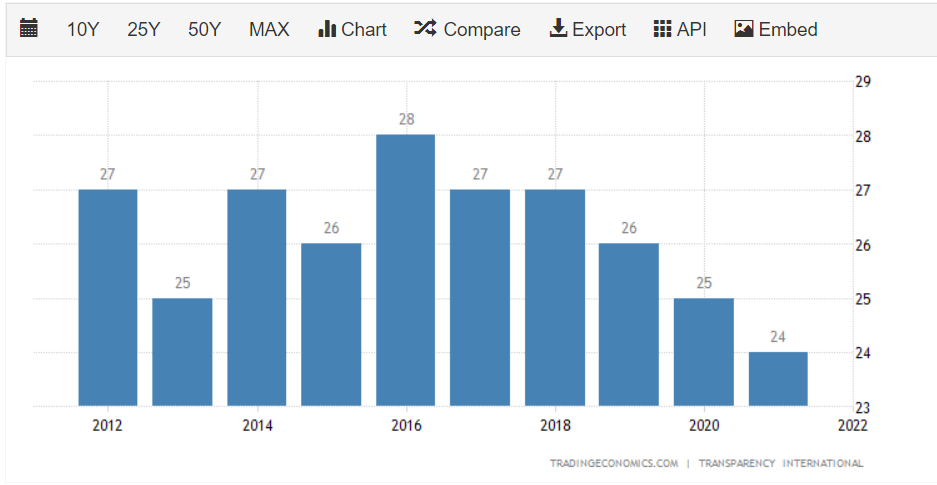
![]() Image 1: Nigeria’s CPI since 2012 (Source: Trading Economics)
Image 1: Nigeria’s CPI since 2012 (Source: Trading Economics)
Is corruption in health a lack of morals or a failure of systems?
Thomas Hobbes described life as nasty and brutish, constantly in a state of war, which explains how the nature of man is disapproving of principles and good behaviour. Hobbes further used this philosophy to buttress the importance of social control (rules and institutions that keep to the demands of the rule of law) against the deviant nature of people and make them more compliant with rules. Just as Hobbes, Sigmund Freud argued that societies get better when the superego (comprising ideals, principles, laws, etc.) is enforced to quell the irrational and socially unacceptable personalities of people (ego). In these, and in other traditional scholarship, the innate tendency to be corrupt appears to be part of human nature, but people can be less or not corrupt in systems that are built to be intolerant of corruption. This is why the Anti-corruption Evidence Consortium argues for the need to strengthen vertical (government offices) and horizontal forces (grassroots people), such that systems can become self-enforcing against corruption.
Therefore, corruption may not entirely be the moral failure of individuals, but even more, a failure of institutions that creates incentives for corrupt practices. At times, institutions may fail to the extent that corruption becomes the only way for people to survive and support their families. Thus, instead of just identifying and punishing individuals who break the rules, an anticorruption agenda must seek to make corruption unattractive and difficult to perpetuate, and at the same time, build a system that can be self-enforcing against corruption.
A reminder about Nigeria’s health sector corruption
A recent review on health sector corruption and a nominal group technique with frontline health workers and policymakers in Nigeria revealed the most common forms of health sector corruption, which were absenteeism, informal payments, health financing corruption, employment irregularities, diversion of patients from public to private facilities, theft of consumables, and illicit procurement practices. More focused research approaches using ethnography, interviews, and group discussions have also shown that the Nigerian health sector is truly challenged by corruption, devastatingly affecting Nigeria’s progress toward achieving global health goals and leading to inefficient use of the current low budgetary appropriations and donor funding to the health sector. The poorest and most disadvantaged groups are most at risk as they have few alternatives to obtain adequate quality care. Indeed, corrupt practices change the ethos of the health system and distort priorities and procedures.
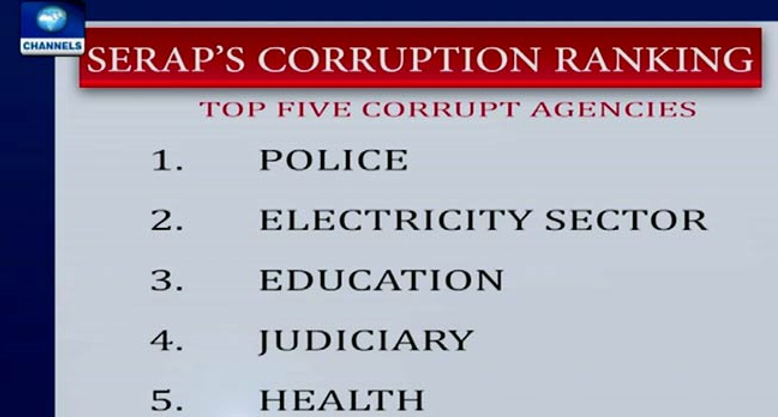
![]() Image 2: Corruption ranking in Nigeria (Source: Channels TV)
Image 2: Corruption ranking in Nigeria (Source: Channels TV)
While the situation often seems helpless, there is hope in the fact that anticorruption can be successful when governance structures are set up and incentivized in ways to gradually curb it, and when grassroots actors finally say, “enough is enough”. Therefore, the question is – how do we stimulate and galvanize the interests and actions of macro governance structures and community actors toward anticorruption in the health sector? Also, how do we ensure that anticorruption approaches do not only work for a period of time but become an integral part of the system and sustainable?
Stakeholders in health sector anticorruption gathered to find solutions
The Health Policy Research Group (HPRG), University of Nigeria and the Bayero University, Kano (BUK), with partnership from the London School of Hygiene and Tropical Medicine (LSHTM) are vigorously pursuing an anticorruption agenda in the health sector of Nigeria through research and the use of evidence from research to inform policies and strategies that will eliminate corruption in the health system. To achieve this goal, the team convened a Policy Forum on Anticorruption in Nigeria tagged “Stop Health Sector Corruption”, attracting various key stakeholders in the Nigerian health system and anticorruption vanguards from several bodies in Nigeria.
Those that were represented included the Independent Corrupt Practices Commission (ICPC), Nigeria Academy of Science (NAS), Health Reform Foundation of Nigeria (HERFON), International Centre for Investigative Reporting (ICIR), Results for Development (R4D), National Health Insurance Scheme (NHIS), Budgit, UNODC, Nigeria Health Watch, Project Pink Blue, Anticorruption Academy of Nigeria, National Primary Health Care Development Agency (NPHCDA), SERVICOM, Nigeria Governors Forum, etc. The stakeholders narrated several personal experiences of health sector corruption and reinforced the urgent importance of addressing this failure.
With several presentations of documented evidence from the research team from UNN and BUK on the realities and dynamics of corruption in Nigeria’s health sector, particularly primary healthcare, the stakeholders confirmed that thoroughness of the research already done by the team, even though they pointed more areas to cover. Strong emphases were made on the managerial components of the health sector, as corruption, unaccountability, and sheer incompetence at that level have allowed for the thriving of corruption and accountability issues at the level of service delivery. The weakness of the Human Resource (HR) component of the public sector, as well as the lack of properly communicated context-specific rules and regulations for the health sector, were considered enablers of corruption.

![]() Image 3: Cross-section of policy forum attendees
Image 3: Cross-section of policy forum attendees
Where do we go from here?
The stakeholders who attended the Policy Forum were clear on where to begin to address health sector corruption. Unanimously, they emphasized the need to drive solutions using evidence from research. Implying that more conversations between researchers in corruption studies and policymakers should be encouraged. Also, based on the reported evidence, stakeholders opined that anticorruption will be unsustainable if strategies do not emanate and include actors at the frontline and those that are affected. It is more like tying the ends of macro politics (the big ‘P’) that comprise the managers at the authority level and their political networks in local government and beyond, with those of micro politics (the small ‘p’) comprising community actors and frontline health workers.
It was for instance suggested that a ‘Rule book’ on anti-corruption in health should be developed and deployed across the country, and civil society groups and community leaders should be encouraged and incentivized to play supportive supervision roles across health facilities. An important incentivization as mentioned by the policymakers is to ensure that the top-level managers act on reports tendered to them by community actors and civil groups. Such is needed for confidence building and developing trust across the “big” (P) and “small” (p) pees. Also mentioned included rapid digitalization of systems, educating service users on patients’ rights as enshrined in law using townhall meetings and media, establishing and optimizing human resource management across health facilities, and putting together reward mechanisms for committed health workers, to mention but a few.

![]() Image 4: Cross-section of policy forum attendees
Image 4: Cross-section of policy forum attendees
There is hope!
With the coming together of these powerful actors sourced from organisations and circles that are influential within Nigeria’s health system and policy space, a critical mass of people and systems that can drive a sustainable anticorruption agenda in the health sector is feasible. The policy forum attendees have made their commitments to this cause and are optimistic about improved situations within the health sector going forward. Therefore, more strategic and meaningful engagements will continuously hold until anticorruption in the health sector becomes an indispensable part of Nigeria’s health system, and the rule of law rises to becoming self-enforcing by the system.
Conclusion
With the amount of information asymmetry in the health system, where service users are barely aware of expectations, ensuring prominence of the rule of law remains a viable anticorruption strategy. We understand that this may be difficult to achieve in developing climes like Nigeria, where individuals and organisations can be even more powerful than the system. It is for this reason scaling-up and optimizing the awareness and voices of citizens at the grassroots is much needed and an achievable anticorruption agenda. And civil groups and researchers will continue to pursue avenues to hold government actors to account and draw their attention to the pathetic consequences of undermining the rule of law as applied to healthcare. More voices are needed in health sector anticorruption, and the Accountability in Action Research Team is excited at the rapidly growing institutionalization of health sector anticorruption, evidenced by:
-
The Thematic Working Group on Action on Accountability and Anti-corruption for SDGs (TWG AAA) at Health Systems Global, where Prof Obinna Onwujekwe and Prof Dina Balabanova (are Co-Chairs)
-
The proposed African Resource Center for Accountability and Anti-corruption in Health, to be based in Nigeria
-
Forthcoming Global Network for Anti-Corruption, Transparency & Accountability in Health Systems (GNACTA) to be launched by WHO, UNDP and other major development agencies in December 2022.
-
The Nigerian Policy Forum on Accountability and Anti-corruption in the health system
Acknowledgement
Associate Prof Eleanor Hutchinson
Dr Tochukwu Orjiakor
Dr Aloysius Odii
Dr Muktar Gadanya
Dr Maikano Madaki
Pamela Ogbozor
Divine Obodoechi
Accountability and Anti-corruption in Health Project Anti-corruption Evidence Consortium (ACE)



