By Shalom Obi, Osondu Ogbuoji, Wenhui Mao, Minahil Shahid, Gavin Yamey, and Obinna Onwujekwe
In the coming years, about a dozen middle-income countries are expected to transition out of development assistance for health (DAH). This is so because the eligibility criteria set by most multilateral donors are based on income per capita or rise in GDP. However, an increase in income per capita does not necessarily mean a reduction in disease burden. For example, despite an increase in GDP, Nigeria still stands out as very unprepared for the upcoming transition, based on poor health indices, very low domestic financing for health, and poor government commitment to health.
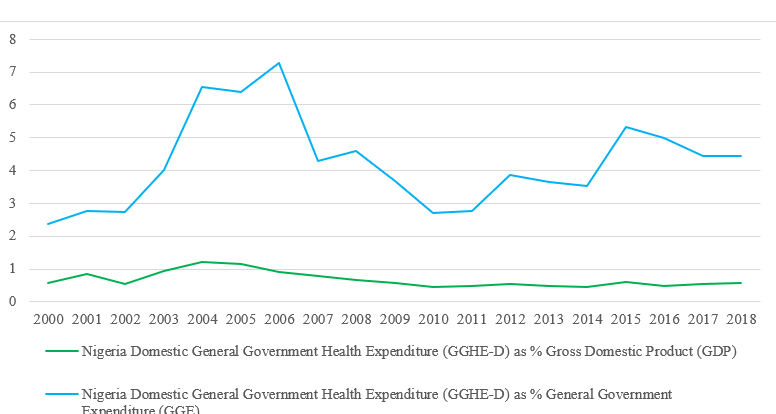
Nigeria is vulnerable to setbacks, in event of health-focused donors exiting its health funding space because the country struggles with a low per capita income, debt burden, weak capacity to efficiently use public resources, limited and less effective health systems, and weak governance and public institutions. More so, considering the low government funding for health (see Figure 1 below), the impending financial gap will most likely shift to out-of-pocket spending which constitutes 75.2% of total health expenditure. This will be catastrophic and may drive more of the vulnerable population below the poverty line. The decline in donor funding has already been reflected in suboptimal service delivery and health service users are now having to pay for previously free-of-charge services.
Figure 1: Trend of Domestic General Government Health Expenditure (GGHE-D) Global Health Expenditure Database
The more currently appropriated funds for health are not subject to high-level accountability, the effects on the vulnerable may likely to be grave, further drawing the country away from achieving UHC. With changes in DAH and impending transitions, there is an urgent need for sustainable solutions, as stakeholders must begin to think about how to fund healthcare when external funds decrease or end.
For evidence-driven transitioning, away from DAH, stakeholders may wish to refer to a qualitative research that used Vogus and Graff’s expanded framework for evaluating the readiness of Nigeria’s transition. Unfortunately, the illustrated gaps (see Figure 2) identified in the study show that Nigeria is not currently prepared to sustain donor-funded programs and make progress if/when donors leave.
Figure 2: Gaps – using Vogus and Graff’s expanded framework for evaluating country readiness for transition of donor-funded health programs to domestic ownership (Vogus and Graff, 2015)
The above framework shows clearly that Nigerian health system is mostly unprepared to transition out of DAH and make progress towards UHC. This is predominantly due to policy implementation gaps, unaccountability and corruption, and a lack of initial transition plans at the onset of health programs.
Policy implication
To overcome the challenges and bottlenecks that hinder policy implementation and close these gaps,
-
Policymakers should consider the feasibility, sustainability, and accountability of policy implementation during the policy process. They should ensure that there are feasible road maps for apt implementation of pro-UHC policies.
-
Secondly, crucial steps must be taken to ensure that transition plans are factored into program planning from the onset, and not as an addendum. A well-grounded health plan that puts transition in perspective is needed to foster sustainability and progress towards UHC at the time of transition.
-
Nigeria must also endeavor to make political commitment to health – at least improve from current 5% of annual budget allocated to the health sector, while racing toward the 15% commitment as promised in the Abuja declaration of 2001. This will enable the country to integrate healthcare programs and build the overall health system to transition smoothly out of various donor programs, whilst making progress towards UHC. Meeting this commitment has become even more critical given the effects of COVID-19 pandemic.
Lessons for upcoming transitioning countries
Upcoming cohort of transitioning countries should have a robust transitioning plan in place to sustain gains of donor funds and make progress toward UHC. Transition plans should not be an afterthought, but a well-incorporated aspect of health programs’ plans. Therefore, donors and recipient countries should ensure that transition plans are built into health programs at the planning stage. Furthermore, it is not enough for upcoming transitioning countries to have pro-UHC policies, they should also have roadmaps for implementation, with broad stakeholder involvement. It is also crucial for such countries to give careful consideration to increasing their fiscal space for domestic funding for health, integration of health programs, and building the overall health system. This will engender sustainability and ensure progress towards UHC at the time of transition. Donors and recipient countries should endeavor to have inbuilt transition plans to give direction to program implementation and enable institutionalization of service delivery processes for continuity.
Conclusively, to manage transitions from DAH and make progress towards UHC, the Nigerian government needs to identify and address implementation gaps, as well as systematic gaps in using domestic resources for financing critical health services. Policymakers should identify clear road maps for the implementation of the existing pro-UHC policies. Furthermore, funds should be redirected to building the overall system—consolidating and coordinating programs and linking them into the overall health system, health financing priorities, and policies. Instead of continuing to invest in parallel programs, a comprehensive and functional structure for continuity, one that will be robust enough to withstand decreasing external funds or donor exits, should be developed at the national and sub-national levels as a matter of urgency.
Shalom Obi is a Research Fellow at the Health Policy Research Group, University of Nigeria, with focus on health policy research and community health systems.
Obinna Onwujekwe is a Professor of Health Economics, Systems and Policies at the University of Nigeria Enugu Campus. He is the Chief Editor of the African Journal of Health Economics, and the Coordinator of the Health Policy Research Group, University of Nigeria. He also coordinates the African Health Observatory Platform (AHOP) for Health Systems, Nigeria Center.
Acknowledgement: We thank Dr Godstime Eigbiremolen for the review of the blog